- The Role of Carbohydrates.
- Glycemic Index Measure.
- Glycemic Index : Observations and Factors.
- Glycemic Load.
- Carbohydrates and Satiety Mechanisms.
- Carbohydrates and Well Being.
- Hypoglycemia.
- Insulin Resistance.
- Sweeteners.
This is the final section of our 3 part series about macronutrients ; this last part is about carbohydrates (you can read the first part about proteins and the second about lipids).
The Role Of Carbohydrates
Carbohydrates, which are sometimes referred to as “sugar”, are molecular compounds, as well as the main energy source for the body.
Carbohydrates are stored inside the muscles as glycogen and inside the liver. An amount is also circulating freely within the bloodstream (as glucose). Glycogen is a complex sugar and an important source of energy.
In spite of what you might have already read, carbohydrates are not an essential nutrient for lifeforms, as opposed to proteins or lipids ; thanks to a process called gluconeogenesis, which is the glucose synthesis from precursors that are not sugars. Gluconeogenesis can be processed from amino acids, lactate, pyruvate and glycerol. Krebs Cycle metabolites can also be converted through gluconeogenesis.
Insulin, which regulates blood sugar, is a hormone secreted by the pancreas, and it pushes into the cells the glucose the organs need. Moreover, insulin stimulates lipogenesis via the acetyl-CoA carboxylase (lipogenesis is a process for lipids synthesis as well as fatty acids synthesis), and it prevents lipolysis from occurring by inhibiting the triacylglycerol lipase.
Insulin is not just a hormone which regulates blood sugar, it is also involved in triglycerides storage (whose synthesis is made from acetyl-CoA) within the adipocytes (which are the fat cells).
Sugar is transported into the cells by insulin, and an amount is directly available in order to produce energy. This energy transport mechanism prevents the fatty acids combustion, thus insulin is called an “antilipolytic hormone”.
Glycemic Index Measure
The glycemic index is a classification which has been established in order to determine the “best” food for human health. The index is based on a reference value of 100 (glucose index). The glycemia was measured on a fasted subject every 30 minutes, for 3 hours (which equals to 6 measurements) after the subject ingested 50 grams of glucose. The area is calculated on the response curve of the triangle:
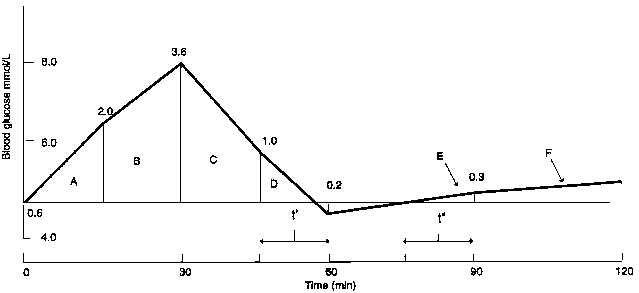
On this triangle, the point A (0.6) corresponds to the glycemia increase, point B to the glycemia peak (3.6), and the last point, C, is the direct glycemia return to its normal value (0.2).
This area is compared to the one obtained from the consumption of pure glucose ; and it allows to precisely obtain the glycemic index of every food. For instance, the area after a banana consumption is 52% inferior to the area which corresponds to the consumption of glucose. Thus, the glycemic index of bananas is 52.
Even though the glycemia increase is not proportional to the amount of carbohydrates that are consumed, many studies underline that the insulin response is correlated to this quantity. It is safe to say the GI of a carbohydrate is a mirror of the insulin response. But this model is limited, because it is possible to end up with two similar areas, yet two very different response curves!
This is the very reason the insulinemic index has been proposed- in order to designate how the body disposes of carbohydrates. Apart from a couple of foods (whey protein for instance), both GI and Insulinemic index are similar.
Glycemic index are generally classified in three categories:
- Low GI when it is inferior or equal to 55.
- Average GI when it is between 56 and 70.
- High GI when it is superior to 70.
Glycemic Index : Observations and Factors
As we saw, the GI measures the bioavailability of the glucose content for a given food, and it is this variability that determines the diversity of the carbohydrate family.
The are many factors which play a role in the GI:
- Starch composition
- Cold or warm consumption
- Protein and lipid content
- Amount of fibre
- Chemical composition (meaning if the food contains glucose, fructose or lactose)
- Maturation degree
- The size of the flour particles
We usually have four families of starches:
- Cereals: wheat, rye, oats, rice, corn, barley
- Legumes: beans, lentils, peas, chickpeas
- Tuberculous: potatoes, sweet potatoes
- Some fruits: bananas, apples, mangoes
There are two components in a starch (solely made of glucose) : amylopectine and amylose, and, depending on the starch, proportions vary.
During the cooking process, gelatinisation happens, which is an inflation by hydration; and this process makes the starch more easily absorbed. To be more precise, the modification of the structure of the starch makes the hydrolysis easier for the enzymes responsible for the absorption of the starch.
Because hydrolysis is facilitated, transformation to glucose happens faster; this leads to an increase of the glycemia, and thus a greater glycemic index. Starches with a poor amylase content lead to an increase glycemic response; for instance potatoes, low in amylose, have a GI of 88, while lentils have an GI of 30.
Moreover, a long cooking time increases the gelatinisation; pasta which has been cooked “Al Dente” has a lower GI than pasta cooked for a longer time. Contrarily, steam cooking reduces this phenomenon. But it is not irreversible! The retrogradation is the opposite process, amylose and amylopectin molecules are reorganized with time and a decrease in temperature; finally a retrograded food is less likely to gelatinize to the same level.
Refrigerated foods which are eaten the day after will have a lower GI than pasta that has just been cooked! Finally, time has an impact in the retrogradation process; some fruits such as bananas contain starches which convert to glucose, and the GI also increases. This is why new potatoes have a lower GI index than regular potatoes.
Lipids slow down glucose absorption and digestion, and this is why high-fat food which also contain carbohydrates have an average GI (such as chocolate).
Fiber slows down absorption and lowers the GI of a food, especially hydrosoluble fibres that you can find in fruits, veggies and some cereals.
Finally, proteins (as gluten) also slow down absorption; this is why breads made of ancient wheat often have a lower GI than breads made with “modern” wheat.
While it can be tempting to think high-GI foods should be avoided, this is not the case. This may be a confusing notion: while the GI helps in determining the “quality” of carbohydrates, it does not help to distinguish between “bad” and “good” foods.
The content of vitamins or minerals, the satiety that comes after the consumption of a food, or even a food’s caloric value are all factors that need to be taken into consideration. This confusion led to the creation of the glycemic load notion.
Glycemic Load
The concept of glycemic load has been proposed in order to bring in more precision: the glycemic increase after the consumption of carbohydrates is not proportional to the amount consumed.
The GI is a good indicator about quality but inaccurate when it comes to the quantity. The glycemic load, which has been created at the Department of Nutrition at the Harvard School is helpful for measuring the GI for a consumed amount.
GL = (GI of a food * consumed amount)/100
Let’s calculate the GL for 200 grams of cooked rice:
- Grams: 200
- Carbohydrates for 100 grams: 26.3
- GI: 43.7
- GL for every gram: 0.218
Watermelon, which has a high GI, contains much water, and there is barely 6 grams of glucose for a 100 gram serving. This means that in order to measure glycemia within the bloodstream, more than 800 grams would be required (in order to obtain 50 grams of glucose), an amount rarely eaten in a classic diet.
The same observation applies for carrots, which have a GI superior to all other vegetables; there is barely 8 grams of carbohydrates for a 100 grams serving. More than 600 grams would thus be required in order to measure the insulin response, another quantity rarely consumed in real life.
The notion of GL is an interesting approach to take in order to have a better idea about the ingestion of a food and it’s insulin response.
Foods with a low GI can have a high GL if a large amount is consumed. For instance, 200 grams of potatoes have a GL which is 3 times higher than the same serving size of lentils ; white rice has a GL superior to the same serving size of potatoes.
Finally, the GL of the bread varies depending on the flour that has been used (white flour or whole grain flour). It is then necessary to consider the GL as a more pertinent measure since it takes into consideration the consumed amount and the GI of a food.
The GI and GL measurements are often used for overweight people, people with insulin resistance or T1 or T2 Diabetics. For people in good health, it may be interesting to talk about glycemia when it comes to satiety mechanisms.
Carbohydrates and Satiety Mechanisms
Sugar alters satiety mechanisms, which are involved in many physiological processes, and also modulates anticipation behaviors. The hunger sensation is triggered by a low level of serum glucose, and this glucopenia (which is a cellular deficit) that corresponds to the depletion of the gastrointestinal supply, triggers the stimulation of some receptors, located into the cortex, the limbic system and the lateral hypothalamus.
There are two kinds of stimuli in these zones:
- Unconditioned stimuli, which are the result of predispositions amongst mammals.
- Conditioned stimuli, created through learning.
The unconditioned stimulus is an attraction for sweet substances, low in salt; this is a common behavior for all mammals.
The conditioned stimulus is made through learning: affinity with savors and food availability. The digestion, the association between a pleasant event and a certain food, or even the idea of a food, are all experiences which are lived for years and which are likely to modulate these affinities (for instance we all recognize the sound of the popping corn and associate it with movies) and set up eating habits.
High GI foods are more likely to disrupt the physiological mechanisms that control satiety in an individual, because they emphasize innate behaviors such as attraction to sugar and the quick digestion that it is associated with.
The feeling of well-being or recompense mechanisms are also stimulated, the notion of pleasure is often higher with these savors, and by association with the sensations we feel, the brain is likely to develop a high attraction in order to reproduce these feelings.
In a fasted state, the body has a couple of mechanisms in order to ensure satiety, such as:
- Neoglucogenesis
- Glycogenolysis
- Energy production via beta-oxidation
- Lipolysis
With the consumption of foods that trigger a high insulin response, the glycemia decreases, as does the energy production from triglycerides or glycogen. This “brake” (the high GI foods) is more likely to increase the feeling of hunger. Finally, we also often consume sweet foods through habit and for pleasure.
All these physiological mechanisms and habits can increase the difficulty for someone to control his/her hunger, and there is a “yo-yo” effect, between the blood glucose regulation and the glycemic levels.
Carbohydrates and Well Being

What is responsible for this feeling of well-being after the consumption of a sweet food? Well, it is mostly the fluctuation of serotonin (5-HTP or 5-Hydroxytryptamine) in the brain. Serotonin is synthesized from L-Tryptophan; this is what creates the feeling of well-being and inner calm. The serotonin effect is antagonist to two others neurotransmitters: dopamine and norepinephrine.
5-HTP synthesis is made possible by the passage of tryptophan through the blood-brain barrier; its penetration is only possible via a common transporter with six others amino acids:
- Leucine.
- Isoleucine.
- Valine.
- Methionine.
- Tyrosine.
- Phenylalanine.
Because of this common transporter (T-Type amino acid transporter), competition occurs for the blood-brain barrier passage. It is interesting to note that the consumption of a high GI food enhances amino acids uptake by muscles; there is then a more important amount of tryptophan that ends up in the brain since the competition with the others amino acids is lessened. This “flash” effect or the feeling of “being high” is directly reproducible by eating insulinogenic foods.
The “yo-yo” effect we talked about earlier can be explained by the circulating levels of serotonin which ends up to be lower than they were before the stimulation which led to the serotonin synthesis.
Chocolate is the best example, not only because is has an important palpability (more than 300 savors), but also because it has an impact on the emotional biochemistry. It is also involved in phenylethylamine synthesis, a monoamine alkaloid from the amphetamines family. Finally, it increases levels of endorphins and anandamide, which are two endogenous neurotransmitters. Chocolate is also a good food during menstruation since it relieves stress and increases well being.
Hypoglycemia
Hypoglycemia is a condition that occurs when your blood sugar (glucose) is too low. It occurs when glycemia is about 0.5 g/l into the bloodstream, but some people feel it even at 0.7g/l.
Foods with a high GL can emphasize this phenomenon, and up to two hours after the consumption of a meal with a high GL, several reactions can occur:
- Hunger sensations.
- Concentration problems.
- Drowsiness.
- Chronic tiredness.
- Vertigo.
The epinephrine response can lead to agressive or nervous behaviors and shakes. Recent studies show that more than 70% of people who have a “modern diet” are concerned by frequent episodes of hypoglycemia.
Hypoglycemia is usually treated with sugar, but this only delays these symptoms that will happen again. A better solution is the consumption of foods with a low GI; this is enough to stabilize blood glucose.
Hypoglycemia, however, is not solely provoked by the consumption of foods with a high GL; some people may be deficient in glucose-6-phosphatase or other enzymes responsible for glucogenesis.
Insulin Resistance
Insulin resistance is the disruption of insulin modus operandi on the concerned tissues, especially the skeletal muscles. The insulin resistance can be genetic: kids with a normal glucose tolerance can develop an insulin resistance if their parents have a T2 Diabetes for instance.
The consumption of high GI food may be responsible for insulin resistance, precisely in the context of a high-fat, high-carbohydrates hypercaloric diet for a long time, which is the precursor to this insulin resistance. Adipocytes around the abdominal zone are the ones concerned by this chronic stimulation ; and it is a common characteristic amongst people suffering from Android Obesity.
For insulin-resistant subjects, this fat cell development leads to the circulation of free fatty acids into the bloodstream, even if insulin (released after the consumption of carbohydrates or proteins) is supposed to prevent the release of these fatty acids. For the muscles, a competition occurs between glucose and fatty acids.
Because muscles will prefer fatty acid oxidation for energy substrates production, Acetyl-CoA will inhibits glycolysis, thus, glycogen storage into muscle cell is slowed down.
Some studies correlated fast twitch fibers (T2 Fibers) and a reduced stimulation through sedentarization and insulin resistance. The fast twitch fibers which are the ones that are stimulated during endurance trainings, and are more prone to insulin resistance than slow twitch fibers (T1 Fibers).
Environment (stress, tobacco, poor sleep conditions) may also play a role in these fat cells repartition. Both stress and alcohol may influence the android distribution of fat cells and age also diminishes the T1 fibers proportion.
Finally, insulin resistance develops when insulin receptors are exhausted. A defective constitution of these cells membrane (due to an insufficient polyunsaturated fatty acids intake, and especially Omega-3) can disrupt the receptors on these cells.
Insulin resistance greatly increases in our societies, and it may be responsible of the “X Syndrome” that associates:
- Obesity.
- Insulin resistance.
- Disrupted lipids metabolism.
- Arterial hypertension.
Cardiovascular diseases and potential T2 diabetes are often correlated to this X syndrome.
Sweeteners

Sweeteners are molecules which do not belong to the family of carbohydrates but which have a high sweetness, usually higher than natural sugar; their caloric content is most of the time irrelevant when they are consumed at normal doses.
For the food industry, sugar is replaced by the following polyols:
- Mannitol (E421).
- Isomalt (E953).
- Maltitol (E965).
- Xylitol (E967).
- Sorbitol (E420).
Because the metabolization mostly occurs into the liver, these polyols are slowly converted to glucose. Generally, these sweeteners (which do not belong to the family of carbohydrates) are used:
- Aspartame (E951).
- Cyclamate (E952).
- Acesulfame (E950).
- Saccharin (E954).
Aspartame
Sweeteners, especially aspartame, are often a subject of discussion, because of their potential effects on human health. Saccharin has been suspected to contain cancer-causing substances, and aspartame can provokes epileptic seizures and brain tumours.
Studies needs to be analyzed with attention; the approval of aspartame for human consumption has known many backs and forths, in France as well as in the United States, by CSAH, AFSSA or the FDA.
For people suffering from hyperinsulinemia, chronic use of aspartame may lead to an increase in cephalic insulin secretions.
Without taking a position, we may nevertheless say some side effects do occur by a chronic use of sweeteners, especially an increased attraction for sweet flavours and similar sensations ; and they could lead to the consumption of foods with a high sugar content.
The numerous so-called “sugar-free” or “diet” foods are more of a marketing apparatus in order to make people believe the food is healthy, but they often have hidden carbohydrates or lipids (such as “sugar-free” chocolate that remains nevertheless high in lipids.)
This notion of “light” may lead to an increased consumption of these foods, thus a possible weight increase as well as chronic hypoglycemia episodes.

